Tap Into a New Possibility
for OCD treatment
Obsessive Compulsive Disorder Can Severely Affect Daily Life
Obsessive Compulsive Disorder (OCD) affects an estimated 2.5 million Americans each year.1 OCD can severely affect daily life, routines, and cause distress or even functional impairment.
Exposure and response prevention (ERP) therapy is typically considered the gold standard treatment for OCD along with adjunctive medication. 50-60% of patients who complete ERP treatment show clinically significant improvement.2
Transcranial magnetic stimulation (TMS) is a safe, proven treatment for depression that can be used for those suffering from OCD when combined with other types of treatment such as medication or behavioral therapy.3
With NeuroStar, All You Have To Do Is Show Up
NeuroStar TMS for OCD is an outpatient treatment that takes only 18 minutes a day for 5 days a week. A full course of treatment totals 29 sessions. During each session, a cushioned coil is precisely placed against your head while magnetic pulses deliver the therapy directly at the source – the brain. Patients can resume regular daily activities right after treatment. NeuroStar is non-invasive and does not share the same common side effects of medications.4,5
Completion Is Key
For best results, it’s important to complete the full number of treatment sessions prescribed by your doctor.

A Drug-free OCD Treatment
NeuroStar helps life become manageable again.
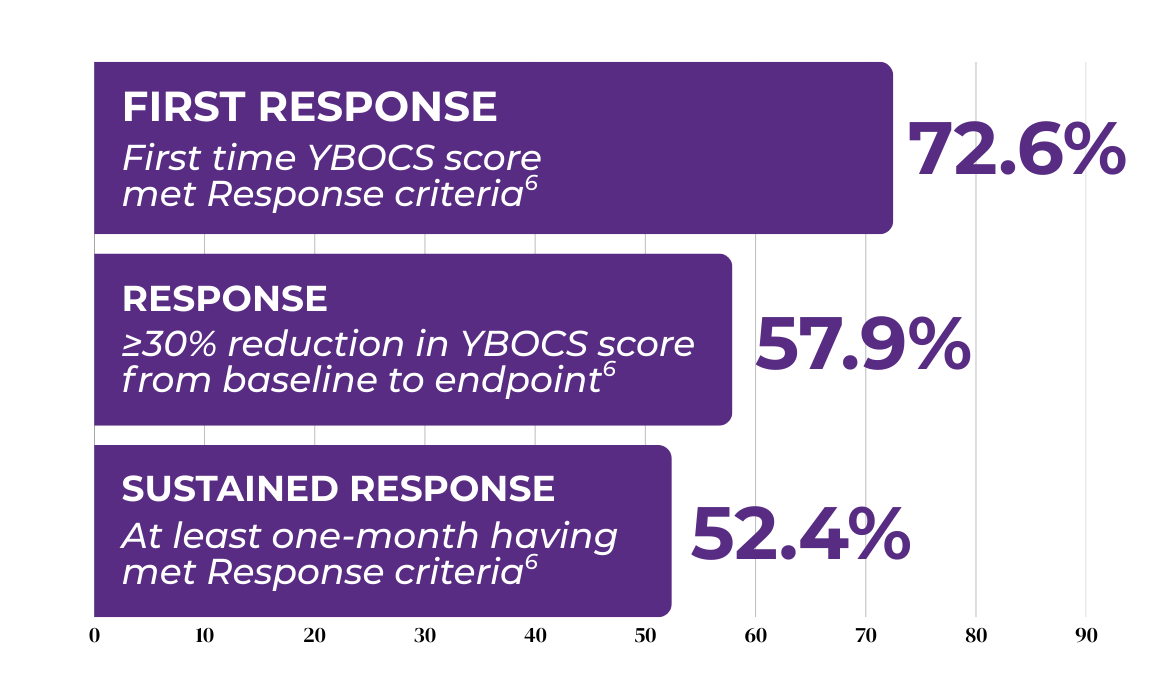
In a published study6, OCD treated with Transcranial Magnetic Stimulation (TMS) has shown improvement in OCD symptoms.
TMS is like physical therapy for the brain. It uses focused magnetic pulses, similar in strength to an MRI, to reignite the synapses in the brain and can provide further relief for OCD symptoms.7,8,9
With NeuroStar, you can live life on your terms.
- Harvard Medical School, 2007. National Comorbidity Survey (NCSSC). (2017, August 21). Retrieved from https://www.hcp.med.harvard.edu/ncs/index.php. Data Table 2: 12-month prevalence DSM-IV/WMH-CIDI disorders by sex and cohort.
- Law C, Boisseau CL. Psychol Res Behav Manag. 2019;12:1167-1174. doi:10.2147/ PRBM.S211117
- Carmi L, Tendler A, Bystritsky A, et al. Am J Psychiatry. 2019;176(11):931-938. doi:10.1176/appi.ajp.2019.18101180.
- NeuroStar. Instructions for Use. Neuronetics, Inc. 2023.
- Janicak PG, O’Reardon JP, Sampson SM, et al. J Clin Psychiatry. 2008;69(2):222-232.
- Roth Y. J Psychiatr Res. 2020; https://doi.org/10.1016/j.jpsychires.2020.11.009
- Post A, Keck ME. J Psychiatr Res. 2001;35(4):193-215.
- Liston C, Chen AC, Zebley BD, et al. Biol Psychiatry. 2014;76(7):517-526.
- O’Reardon JP, Solvason HB, Janicak PG, et al. Biol Psychiatry. 2007;62(11):1208-1216.


